
Last updated: 22-03-2024
Overview
When we talk about migraines, it’s easy to just label them as super headaches.
But, oh, they're so much more than that. Migraines are this whole intense experience that can knock you off your feet, bringing along a whole circus of symptoms that can stick around for what feels like forever – we're talking hours or even days.
The reading time for this article is 12 minutes, we will tell you everything about migraines.
What is a migraine?
Migraine is a complex condition with a genetic basis, leading to episodes of moderate-to-severe headaches. These headaches usually affect one side of the head and are often accompanied by nausea and a heightened sensitivity to light and sound.
The most common type of migraine is without aura (70-75% of cases) (NIIH). Migraines are typically divided into three phases: prodromal, headache, and postdrome.
According to the WHO, slightly less than half of the planet's inhabitants suffer from migraines. This accounts for 3.1 billion people according to the data for 2021.
Symptoms. Check if It's really a migraine
Before the migraine, you may experience prodromal symptoms,
-
extreme fatigue,
-
yawning,
-
cravings for certain foods,
-
thirst, mood changes,
-
a stiff neck,
-
increased urination.
These signs suggest that a migraine attack is imminent.
Migraine headache
When the migraine's main act—the headache phase—kicks in, it comes with a signature set of symptoms that sets it apart from other types headaches.
The primary feature of a migraine headache is a severe, throbbing pain often localized to one side of the head, although it can also affect both sides.
Other common symptoms accompanying the headache phase include:
-
Nausea and vomiting
-
Sensitivity to light and sound:
-
Visual disturbances:
-
Sensitivity to smells:
-
Dizziness or lightheadedness:
-
Scalp tenderness: The skin and scalp may feel sensitive to the touch, making even brushing one's hair painful.
-
A migraine headache can last for several hours to several days.
The intensity and duration of the headache, as well as the presence and severity of other symptoms, can vary significantly from one person to another and from one attack to another.
Important!
If you find these symptoms in you, you can learn more about Reducing Pain Steps or complete an online short medical assessment from Click Pharmacy, or following recommendations from the NHS:
If migraine medication is ineffective, and you feel worse, visit your GP.
Get an urgent GP appointment or call 111 if you:
-
Experiencing jaw pain while eating
-
Blurred or double vision
-
A sore scalp – even gentle brushing feels uncomfortable.
-
Other peculiar sensations, like numbness or weakness in the arms or legs.
If your symptoms or your child's symptoms worsen, consider the cases from the NHS in which you need to urgently call for help on 999.
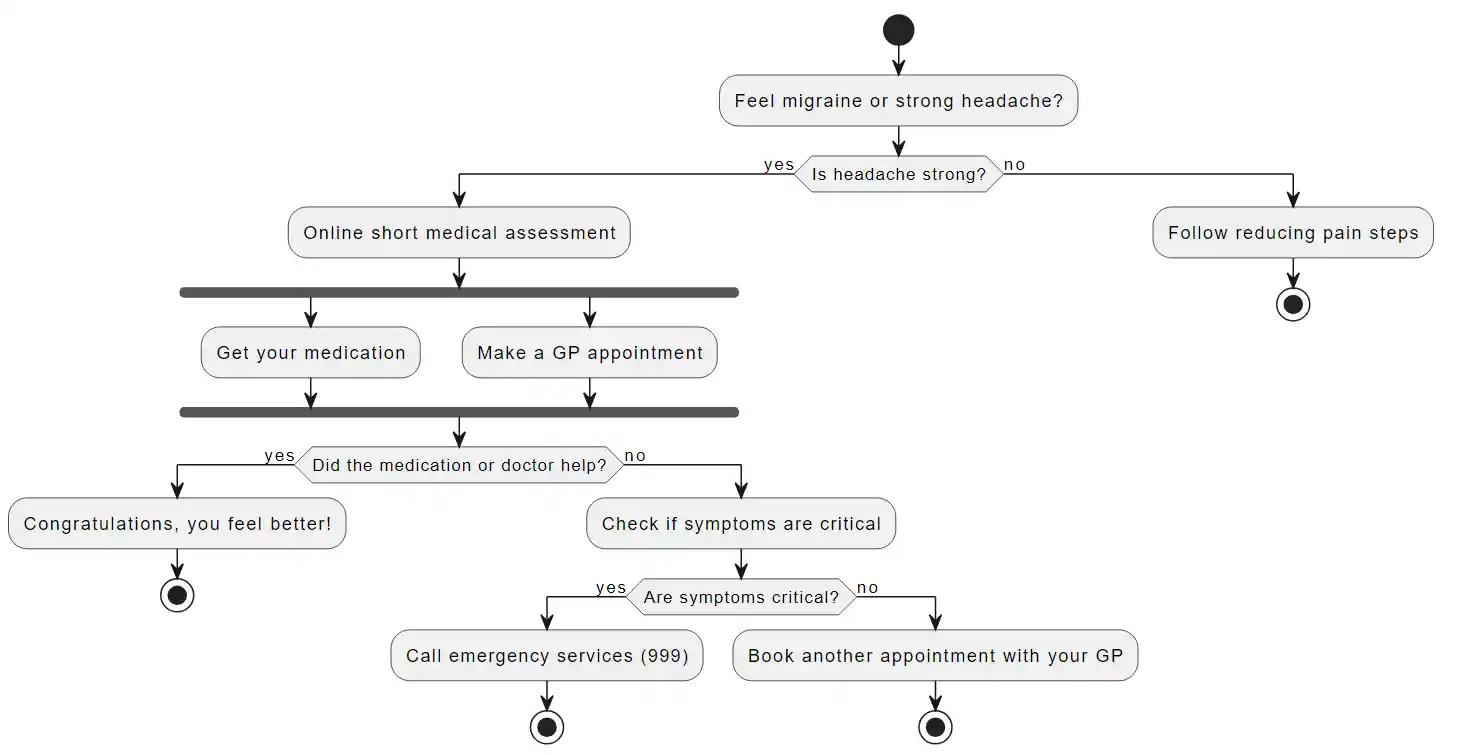
Your migraine action plan looks as follows:
Migraine Postdrome
We recommend reading our article on postdrome insights into migraines. In short, the symptoms of a migraine hangover can vary but often include:
-
Fatigue and lethargy: A profound sense of exhaustion is common.
-
Cognitive difficulties: Problems with concentration and processing information.
-
Mood changes: Feelings of light depression or euphoria.
-
Physical discomfort: Stiff neck, sensitivity to light, and dizziness.
Therefore, when you feel relief from the headache, but have these feelings, know that they can last from a few hours in most cases up to 24 hours to more than a day. And this is the Postdrome phase.
Migraine Types
Grasping the various types of migraines is essential for their effective management and treatment. Here’s a clear-cut consultation on the subject:
-
Migraine without aura, affecting approximately 70-75% of migraine sufferers, is the most common type of migraine. Source: American Migraine Foundation
-
Migraine with Aura, Characterized by neurological symptoms such as visual disturbances and tingling before the headache.
-
Chronic Migraine, Defined by headaches occurring on 15 or more days per month, with migraines on at least eight of those days.
-
Menstrual Migraine, Occurs in relation to the menstrual cycle, often starting two days before to three days after menstruation begins, due to hormonal fluctuations.
-
Hemiplegic Migraine, A rare type involving temporary paralysis or weakness on one side of the body, along with other symptoms.
-
Abdominal migraine, is a subtype of migraine that primarily affects children. It is characterized by episodes of moderate to severe abdominal pain, which can last from one to 72 hours.
-
Vestibular Migraine, Leads to dizziness and balance issues, representing the neurological disorder's impact beyond pain.
You can determine your type of migraine, and based on your type, refer to our online short medical assessment or to your GP with a clear question about migraines. This way, you can better understand what has happened to you.
Migraine Causes and Triggers
If you've asked yourself what the cause of my migraine is, let's look at the main causes of migraines that are known to us.
Сauses of migraines are multifaceted, involving a combination of genetic, environmental, and physiological factors. Here’s a comprehensive overview:
-
Genetic Factors Migraines have a strong genetic component, with many sufferers having a family history of the condition.
-
Environmental Triggers, These triggers vary among sufferers but commonly include stress, hormonal changes (such as those related to menstruation in women), certain foods and additives.
-
Physiological Changes, Migraine attacks are believed to be initiated by a cascade of neurological and biochemical events. If you don't see other reasons, we recommend considering Physiological Changes specifically.
-
Neurotransmitter Imbalance, Serotonin, a key neurotransmitter in the brain, is closely linked to migraines. Changes in serotonin levels can affect the blood vessels in the brain. It would not be harmful to check your Serotonin level in the blood.
-
Central Nervous System Disorders. Issues in specific parts of the brain, like the overly sensitive cerebral cortex and problems in the brainstem that controls pain, also play a role in causing migraines.
-
Lifestyle and Behavioral Factors, Lack of sleep, dehydration, skipped meals, or poor diet can also trigger migraines in some individuals. Managing these lifestyle factors can help reduce the frequency and severity of migraine attacks.
Migraine Treatments
Migraine Treatments is a large section that is divided into many different categories such as medications against migraines, for preventive treatment of migraines, and non-medical steps for treatment. Medication relief for migraines is an effective solution in treatment, but we recommend first consulting a specialist to choose the best treatment specifically for you.
Frequently Asked Questions
Is migraine dangerous?
Migraines are typically not dangerous but can significantly affect the quality of life. Rarely, they can be associated with more serious conditions, like stroke or aneurysms, in very specific cases.
Can a migraine last a week?
Yes, in some cases, a migraine can last for a week or more, which is referred to as status migrainosus. This requires medical attention.
Can migraine be a sickness?
Yes, migraine is considered a neurological condition characterized by intense headache episodes and other symptoms like nausea, light sensitivity, and visual disturbances.
Can cocoa cause migraines?
Some people may find that cocoa or chocolate triggers their migraines, though it can vary from person to person. Cocoa contains caffeine and other compounds that can influence migraines.
How long do migraines last?
Migraine attacks can last for 4 to 72 hours if untreated. The frequency and duration can vary greatly among individuals.
Why do migraines happen?
Migraines can occur due to a combination of genetic, environmental, and neurological factors. Triggers can include stress, certain foods, hormonal changes, and sensory stimuli.